|

by Karen Foster
September 27, 2013
from
PreventDisease Website
|
Karen
Foster
is a holistic nutritionist, avid blogger, with five
kids and an active lifestyle that keeps her in
pursuit of the healthiest path
towards a life of
balance. |
Trillions of bacteria are hostile and can cause disease, while many
others are friendly and have established a symbiotic, mutually
beneficial relationship with us over the millennia.
These friendly bacteria have also been
referred to as "probiotics"
and are being used increasingly by mainstream clinicians for both
preventive and therapeutic purposes. The literal translation of the
word probiotic is "for life."
A growing number of studies suggest that
part of what determines how the human body functions may be not only
our own genes, but also the genes of the trillions of microorganisms
that reside on and in our bodies.
Bacteria
Keep Us Alive
The genomes of the bacteria and viruses of the human gut alone are
thought to encode 3.3 million genes.
"The genetic richness and complexity
of the bugs we carry is much richer than our own," says Jayne
Danska, an immunologist at the Hospital for Sick Children
Research Institute in Ontario, Canada.
"They serve as a buffer and
interpreter of our environment. We are chimeric organisms."
Problems ranging from autoimmune disease
to clinical depression and simple obesity may in fact be linked to
immune dysfunction that begins with a "failure to communicate" in
the human gut, scientists say.
Health care of the future may include
personalized diagnosis of an individual's "microbiome" to determine
what prebiotics or probiotics are needed to provide balance.
A role for gut microbes in gastrointestinal function has been well
documented since researchers first described differences in the
fecal bacteria of people with inflammatory bowel disease The
molecular mechanisms responsible for the gut microbiome's impact on
metabolism and diseases throughout the body remain largely unknown.
However, researchers are beginning to
decipher how the microorganisms of the human intestinal tract
influence biological functions beyond the gut and play a role in
immunological, metabolic, and neurological diseases.
"Asked about their immune system,
most people might think of white blood cells, lymph glands or
vaccines," said Dr. Natalia Shulzhenko, author of a new report
in Clinical Reviews in Allergy and Immunology, and
assistant professor and physician in the OSU Department of
Biomedical Sciences.
"They would be surprised that's not
where most of the action is. Our intestines contain more immune
cells than the entire rest of our body."
Early research on microbiota focused
largely on the commensal bacteria that reside in the human gut.
Commensal gut bacteria supply nutrients,
help metabolize indigestible compounds, and defend against
colonization by nonnative opportunistic pathogens.
The Good and The
Bad
But the distinction between "good" microbes that aid health and
"bad" pathogenic microbes that cause disease has become blurred in
recent years.
Researchers have shown that under
certain conditions, some types of normal gut bacteria can trigger
disease.
Sarkis Mazmanian, a
microbiologist at the California Institute of Technology, dubbed
these elements "pathobionts"; the term "pathogens," in contrast,
refers to
opportunistic microbes that are not normally
part of the gut microbial community.
Disturbances to the microbial
equilibrium of the gut may mean that some microbes become
overrepresented while others are diminished.
"It's like a garden - you're less
likely to have weeds growing if you have lush vegetation, but
without this vegetation the weeds can potentially take over,"
Mazmanian says.
When the gut moves toward a state of
microbial imbalance, normally benign gut microbes may begin to
induce inflammation and trigger disease throughout the body, even in
the nervous system.
Researchers have long postulated that gut bacteria influence brain
function. A century ago, Russian embryologist Elie Metchnikoff
surmised that a healthy colonic microbial community could help
combat senility and that the friendly bacterial strains found in
sour milk and yogurt
would increase a person's longevity.
In 2011 Mazmanian and colleagues
reported that changes in gut
microbial composition might have far-ranging effects that extend to
the brain.
Mazmanian says, the microorganisms that colonize the human gut don't
leave the intestine, but the immune cells that contact them do. He
explains that, although 70% of the immune cells in the body at any
one time can be found in the intestine, they circulate throughout
the body, and the microbiota of the gut environment help determine
how immune cells will behave elsewhere.
He gives an example:
"If T-cells, while in the gut, are
programmed by the microbiota to have anti-inflammatory
properties, then they may suppress inflammation even after they
leave the gut."
Proteins, carbohydrates, and other
molecules shed by microbes also leave the gut and may play a role in
signaling disease. Studies have shown these bacterial metabolites
are pervasive throughout the body - in the lungs, amniotic fluid,
and breast milk, all tissues once thought to be free of microbial
communities.
Other researchers have suggested a link
between the gut - brain axis and neuropsychiatric disorders such as
autism, depression, and eating disorders.
The gut contains microorganisms that
share a structural similarity with the neuropeptides involved in
regulating behavior, mood, and emotion - a phenomenon known as
molecular mimicry.
The body can't tell the difference
between the structure of these mimics and its own cells, so
antibodies could end up attacking both, potentially altering the
physiology of the gut - brain axis.
The Power
of Probiotics
Probiotics offset other intestinal bacteria that produce
putrefactive and carcinogenic toxins.
If harmful bacteria dominate the
intestines, essential vitamins and enzymes are not produced and the
level of harmful substances rises leading to cancer, liver and
kidney disease, hypertension, arteriosclerosis and abnormal
immunity.
Harmful bacteria can proliferate under
many different circumstances including,
The best known of the probiotics are the
Lactobacilli, a number of species
of which (acidophilus, bulgaricus, casei and sporogenes) reside in
the human intestine in a symbiotic relationship with each other and
with other microorganisms (the friendly Streptococci, E. coli and
Bifidobacteria).
Lactobacilli are essential for
maintaining gut microfloral health, but the overall balance of the
various microorganisms in the gut is what is most important.
Another probiotic which has recently generated a great deal of
interest is the friendly yeast known as Saccharomyces boulardii, an
organism that belongs to the Brewer's Yeast family, not the Candida
albicans group. S. boulardii is not a permanent resident of the
intestine but, taken orally, it produces lactic acid and some B
vitamins, and has an overall immune enhancing effect.
In fact, it has been used
therapeutically to fight candida infections.
6
SURPRISING FACTS ABOUT MICROBES IN YOUR GUT
-
What's in Your Gut May Affect
the Size of Your Gut
Need to lose weight? Why
not try a gut bacteria transplant?
New research published in the
journal
Science
suggests that the microbes in your gut may play a role in
obesity.
-
Probiotics May Treat Anxiety and Depression
Scientists have been exploring the
connection between gut bacteria and chemicals in the brain
for years. New research adds more weight to the theory that
researchers call "the microbiome - gut - brain axis."
Research published in
Proceedings of the National Academy of Science
shows that mice fed the bacterium Lactobacillus
rhamnosus showed fewer symptoms of anxiety and
depression. Researchers theorize that this is because L.
rhamnosus acts on the central gamma-aminobutyric acid (GABA)
system, which helps regulate emotional behavior.
L. rhamnosus,
which is available as a commercial probiotic supplement, has
also been linked to the prevention of diarrhea, atopic
dermatitis, and respiratory tract infections.
-
The More Bacteria the Better
While bacteria on the outside of your
body can cause serious infections, the bacteria inside your
body can protect against it. Studies have shown that animals
without gut bacteria are more susceptible to serious
infections.
Bacteria found naturally inside
your gut have a protective barrier effect against other
living organisms that enter your body. They help the body
prevent harmful bacteria from rapidly growing in your
stomach, which could spell disaster for your bowels.
To do this, they develop a
give-and-take relationship with your body.
-
Gut Bacteria Pass from Mother to Child in
Breast Milk
It's common knowledge that a mother's
milk can help beef up a baby's immune system. New research
indicates that the protective effects of gut bacteria can be
transferred from mother to baby during breastfeeding.
Work published in
Environmental Microbiology shows that
important gut bacteria travels from mother to child through
breast milk to colonize a child's own gut, helping his or
her immune system to mature.
-
Lack of Gut Diversity Is Linked to Allergies
Too few bacteria in the gut can throw the immune system off
balance and make it go haywire with hay fever.
Researchers in Copenhagen
reviewed the medical records and stool samples of 411
infants. They found that those who didn't have diverse
colonies of gut bacteria were more likely to develop
allergies.
But before you throw your gut
bacteria a proliferation party, know that they aren't always
beneficial.
-
Gut Bacteria Can Hurt Your Liver
Your liver gets 70 percent of its
blood flow from your intestines, so it's natural they would
share more than just oxygenated blood.
Italian researchers
found that between 20 and 75 percent of
patients with chronic fatty liver disease - the kind not
associated with alcoholism - also had an overgrowth of gut
bacteria.
Some believe that the transfer
of gut bacteria to the liver could be responsible for
chronic liver disease.
How Do
Probiotics Work
Probiotics work in many different
ways by their production of antimicrobial substances (organic
acids, hydrogen peroxide, and bacteriocins) that inhibit
pathogen adhesion and degrade toxins produced by microbial
invaders.
Probiotics resist colonization by
competing for binding sites as well as for nutrients with
pathogens. In other words, they crowd out pathogens like candida
and harmful E. Coli.
Probiotics secrete various proteins that stimulate the immune
system both locally and throughout the body, boost intestinal
brush border enzyme activity and increase secretory-IgA (a
family of antibodies lining mucous membranes).
Enzymes like,
-
lactase
-
sucrase
-
maltase
-
alpha-glucosidase
-
alkaline phosphatase,
...are enhanced by probiotics.
Cholesterol and triglyceride blood levels are metabolized and
lowered by healthy probiotic populations.
Probiotics are able to resist
translocation, defined as the passage of pathogens from the GI
tract to extraintestinal sites such as the mesenteric lymph node
(MLN), spleen, liver, kidneys, and blood.
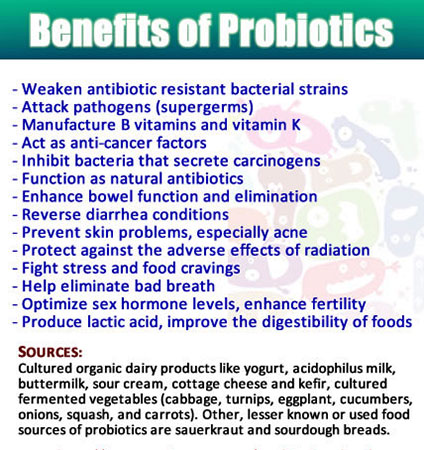
Benefits of
Probiotics
The following are the most well
documented benefits of taking probiotics regularly:
-
Weaken antibiotic resistant
bacterial strains, attack new types of pathogens (supergerms)
and infections in immuno-compromised people requiring
treatment (i.e. resist opportunistic infections like
candidiasis)
-
Manufacture B vitamins
(biotin, B3, B5, B6, folic acid, B12) and vitamin K
-
Secrete lactase, an enzyme
required to break down lactose in milk
-
Act as anti-cancer factors
(especially for bladder and bowel) by inhibiting
bacteria that convert nitrates into nitrites
-
Inhibit bacteria that
secrete carcinogens
-
Function as natural
antibiotics against unfriendly bacteria, viruses and
yeast like Candida albicans
-
Enhance bowel function and
elimination; prevent constipation
-
Reverse diarrhea conditions
(Crohn's disease, AIDS, Traveller's)
-
Reduce or eliminate
bloating, gas, straining and abdominal pain due to any
cause
-
Prevent skin problems,
especially acne and other skin infections. (FYI - most
chronic acne conditions in adults are often improved or
eliminated by a good bowel flora balance).
-
Protect against the adverse
effects of radiation and pollutants
-
Reduce blood levels of
cholesterol and triglycerides
-
Fight stress and food
cravings and thereby prevent or reverse obesity
-
Help eliminate bad breath
-
Optimize sex hormone levels,
enhance fertility and prevent osteoporosis
-
Produce lactic acid, improve
the digestibility of foods
-
Oppose putrefactive bacteria
like bacteroides associated with a meat-rich diet
-
Treat eczema, psoriasis,
ulcerative colitis, Crohn's Disease, irritable bowel
syndrome, all cancers, gastritis, duodenitis,
diverticulitis, food allergies, lactose intolerance,
environmental allergies, urinary tract infections,
vaginitis, other chronic infections (TB, AIDS, Herpes,
venereal diseases) and autoimmune diseases (e.g.
rheumatoid arthritis, polymyalgia rheumatica, ankylosing
spondylitis, psoriasis, lupus, alopecia areata,
scleroderma, thyroiditis, etc.)
Probiotic Sources
Cultured dairy products like,
-
yogurt
-
acidophilus milk
-
buttermilk
-
sour cream
-
cottage cheese
-
kefir,
...are the best known food
sources of friendly bacteria.
Equally effective probiotic food
sources include
cultured/fermented vegetables
(cabbage, turnips, eggplant, cucumbers, onions, squash, and
carrots). Other, lesser known or used food sources of
probiotics are sauerkraut and sourdough breads.
Ideally, one could get a good
supply of probiotics from one or more of these diverse
foodstuffs. If dietary sources are not easily available,
supplemental probiotic powders and capsules are good
alternatives.
Choose a brand that has at least
3 different strains of friendly bacteria and between 6 - 15
billion live organisms.
Sources
|